Glaucoma is a serious eye condition that affects millions of people worldwide. It can lead to vision loss and even blindness if left untreated. In addition to glaucoma, there are several retinal diseases that can also impact your vision. Understanding the connection between these two conditions is crucial in protecting your vision and exploring treatment options such as glaucoma surgery.
Understanding Glaucoma and Retinal Diseases
The eye is a complex organ, comprised of several structures working together to provide visual perception. To better understand glaucoma and its relationship with retinal diseases, it is important to grasp the anatomy of the eye and the functions of different components.
When it comes to managing vision loss caused by glaucoma and retinal diseases, surgery can be a viable treatment option. Glaucoma surgery aims to lower intraocular pressure and preserve vision by improving the drainage of fluid within the eye.
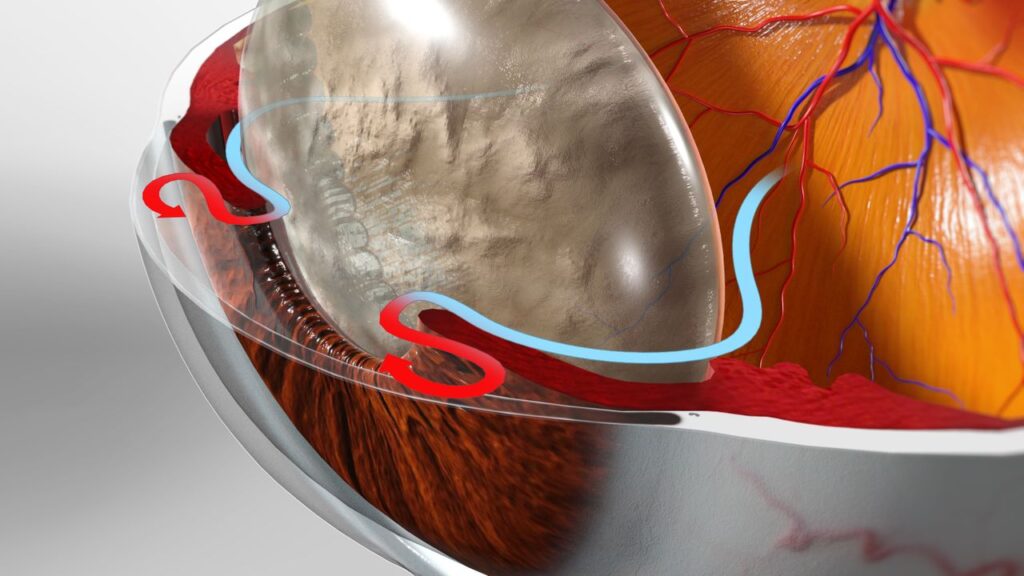
The Anatomy of the Eye
The eye consists of various parts, including the cornea, iris, lens, retina, and optic nerve. The cornea acts as a protective layer at the front of the eye, while the iris controls the amount of light that enters the eye. The lens focuses light onto the retina, which is a thin layer of tissue located at the back of the eye. The retina contains specialized cells called photoreceptors, specifically rods and cones, which convert light into electrical signals that are then sent to the brain via the optic nerve. This intricate process is essential for vision and allows us to perceive the world around us in vibrant detail.
Moreover, the retina is not just a passive receiver of light; it also plays a crucial role in visual processing. The macula, a small but highly sensitive area in the center of the retina, is responsible for detailed central vision and color perception. This region is vital for tasks such as reading, driving, and recognizing faces, highlighting the significance of retinal health in maintaining clear eyesight.
What is Glaucoma?
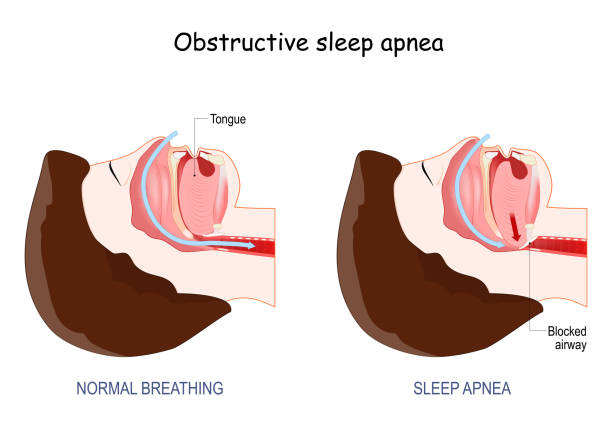
Glaucoma is a group of eye diseases that damage the optic nerve, often due to increased pressure in the eye. This increased pressure, known as intraocular pressure, can occur when the fluid inside the eye does not drain properly. As a result, the optic nerve becomes damaged, leading to vision loss. Glaucoma is often referred to as the “silent thief of sight” because it can progress slowly and without noticeable symptoms until significant vision loss has occurred. Regular eye exams are crucial for early detection and management of this condition.
Common Retinal Diseases
In addition to glaucoma, there are various retinal diseases that can affect your vision. Some common retinal diseases include age-related macular degeneration (AMD), diabetic retinopathy, and retinal detachment. Age-related macular degeneration is a leading cause of vision loss in older adults, affecting the central vision and making activities like reading and driving challenging. Diabetic retinopathy, on the other hand, is a complication of diabetes that can cause damage to the blood vessels in the retina, leading to vision impairment. Retinal detachment is a serious condition where the retina pulls away from its normal position, requiring prompt medical attention to prevent permanent vision loss. Read more about diabetic retinopathy on https://www.ncbi.nlm.nih.gov/books/NBK560805/
The Connection Between Glaucoma and Retinal Diseases
While glaucoma primarily affects the optic nerve, it can also impact the retina, which is responsible for capturing and processing visual information. The relationship between glaucoma and retinal diseases is complex and multifaceted.
Glaucoma causes damage to the optic nerve, but it can also lead to changes in the retina. As the optic nerve is responsible for transmitting information from the retina to the brain, any damage to the optic nerve can disrupt this flow of information and result in vision impairment.
Furthermore, the impact of glaucoma on the retina can manifest in various ways. In some cases, glaucoma can cause thinning of the retinal nerve fiber layer, which can be detected through specialized imaging techniques like optical coherence tomography (OCT). This thinning of the nerve fiber layer can result in visual field defects, affecting peripheral vision and potentially progressing to central vision loss over time.
Retinal Diseases that can Lead to Glaucoma
On the other hand, certain retinal diseases can increase the risk of developing glaucoma. For instance, conditions like diabetic retinopathy and retinal detachment can lead to changes in eye fluid dynamics, causing an increase in intraocular pressure and subsequently increasing the likelihood of glaucoma development.
Diabetic retinopathy, a common complication of diabetes, can result in the growth of abnormal blood vessels in the retina. These abnormal blood vessels can lead to neovascular glaucoma, a type of secondary glaucoma characterized by the formation of new, fragile blood vessels on the iris that block the normal flow of eye fluid. This blockage can increase intraocular pressure, contributing to optic nerve damage and vision loss if left untreated. To read more about fragile blood vessels click here.
The Importance of Early Detection
Early detection of both glaucoma and retinal diseases is crucial in preventing further damage to your vision. Being aware of the symptoms associated with these conditions and regularly visiting an eye care professional can help catch any issues at an early stage.
Glaucoma is often referred to as the “silent thief of sight” because it can progress without noticeable symptoms until significant vision loss has occurred. On the other hand, retinal diseases like age-related macular degeneration (AMD) can cause a gradual loss of central vision over time. By detecting these conditions early, treatment options can be more effective in preserving your eyesight.
Symptoms to Watch Out For
While glaucoma and retinal diseases can often progress silently, there are some common symptoms to watch out for. These may include blurred vision, difficulty seeing in low light conditions, blind spots in the visual field, and sudden changes in vision. If you experience any of these symptoms, it is important to seek immediate medical attention.
In addition to the symptoms mentioned above, individuals with glaucoma may also experience eye pain, headaches, nausea, and halos around lights. Retinal diseases, on the other hand, can manifest as distortions in straight lines or a decrease in color perception. Recognizing these signs early on can lead to prompt diagnosis and management of these sight-threatening conditions.
Regular Eye Examinations and Their Role
Regular eye examinations play a vital role in the early detection of eye conditions. During these exams, your eye care professional will evaluate the health of your retina and optic nerve, as well as measure your intraocular pressure. These routine screenings can help identify any signs of glaucoma or other retinal diseases before they progress.
Furthermore, eye examinations can also detect systemic conditions such as diabetes and hypertension, which may have ocular manifestations. By monitoring your eye health regularly, you not only safeguard your vision but also contribute to the overall assessment of your well-being.
Glaucoma Surgery as a Treatment Option
Glaucoma is a group of eye conditions that damage the optic nerve, often due to increased pressure in the eye. If left untreated, glaucoma can lead to irreversible vision loss. Surgery becomes necessary when other treatments, such as eye drops or laser therapy, are not effective in controlling the progression of the disease.

Different Types of Glaucoma Surgery
There are various types of glaucoma surgery, each designed to address specific aspects of the condition. Some common procedures include trabeculectomy, in which a small drainage channel is created to reduce intraocular pressure, and tube shunt surgery, which involves implanting a tiny tube to redirect fluid flow. Learn more advanced glaucoma technique on: Advanced Glaucoma Surgery Techniques
In addition to these procedures, newer minimally invasive glaucoma surgeries (MIGS) have been developed in recent years. MIGS techniques use microscopic-sized equipment and tiny incisions to reduce intraocular pressure with fewer complications and faster recovery times compared to traditional surgeries.
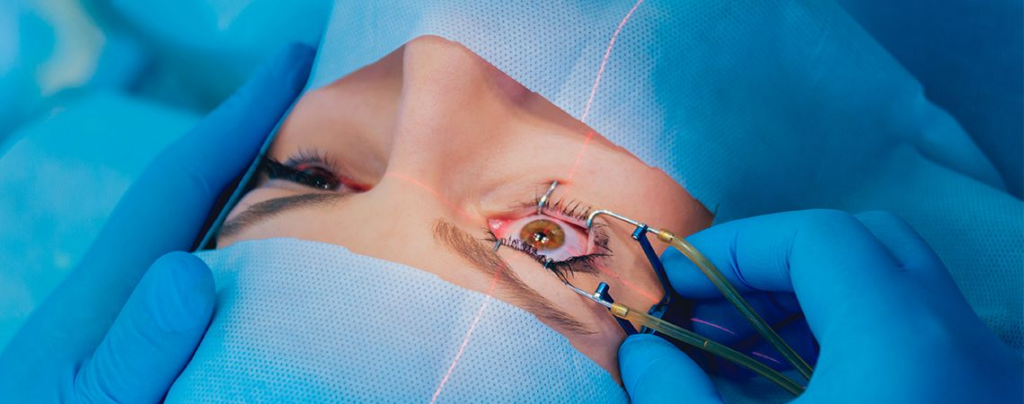
The Process of Glaucoma Surgery
Glaucoma surgery typically involves several steps. First, the eye is numbed with local anesthesia. Then, an incision is made to access the drainage structures. The surgeon will then perform the necessary modifications to improve fluid outflow. Finally, the incision is closed, and the eye is allowed to heal.
After surgery, patients may experience some discomfort, blurred vision, or sensitivity to light. It is essential to follow post-operative care instructions provided by the ophthalmologist to ensure proper healing and optimal results.
Risks and Benefits of Glaucoma Surgery
As with any surgical procedure, glaucoma surgery carries certain risks and benefits. While the surgery can effectively lower intraocular pressure and slow down the progression of glaucoma and retinal diseases, there is also the possibility of complications such as infection, bleeding, and inflammation. It is important to discuss the potential risks and benefits with your eye care professional before making a decision.
Ultimately, the goal of glaucoma surgery is to preserve vision and improve the quality of life for individuals affected by this sight-threatening condition. By exploring all treatment options and working closely with your eye care team, you can make informed decisions about the best course of action for managing your glaucoma effectively.
Post-Surgery Care and Management
After undergoing glaucoma surgery, proper post-operative care and management are essential for a successful recovery and long-term maintenance of vision.
Ensuring that you follow your surgeon’s post-operative care instructions diligently can significantly impact the outcome of your surgery. This includes properly administering any prescribed medications, adhering to the recommended schedule for eye drops, and being mindful of any restrictions on activities during the initial healing phase. By taking these measures seriously, you are actively contributing to the success of your recovery process and the preservation of your eyesight.
What to Expect After Glaucoma Surgery
After glaucoma surgery, your eye may be covered with a protective shield or bandage for a short period. You may experience some discomfort, mild pain, or temporary blurred vision. It is important to follow your surgeon’s instructions regarding medication, eye drops, and any necessary restrictions on activities during the healing process.
Additionally, it is common to experience some redness or swelling in the eye following surgery. This is a normal part of the healing process and should subside over time. If you have any concerns about the level of pain or discomfort you are experiencing, do not hesitate to contact your healthcare provider for guidance and reassurance.
Long-Term Management and Follow-Up
Following glaucoma surgery, regular follow-up appointments with your eye care professional are crucial. These visits allow your surgeon to monitor your eye health, assess the success of the surgery, and make any necessary adjustments to your treatment plan. It is important to attend these appointments and communicate any changes or concerns regarding your vision.
Furthermore, maintaining a healthy lifestyle can also contribute to the long-term success of your glaucoma surgery. Factors such as a balanced diet, regular exercise, and avoiding smoking can positively impact your overall eye health and potentially slow down the progression of the disease. By incorporating these habits into your daily routine, you are actively supporting the effectiveness of your treatment and the well-being of your eyes.
Protecting your vision is of utmost importance, especially when dealing with conditions like glaucoma and retinal diseases. By understanding the connection between these conditions and exploring treatment options such as glaucoma surgery, you can take proactive steps towards preserving your vision and maintaining a healthy lifestyle. Remember to prioritize regular eye examinations and seek professional advice for personalized recommendations and guidance.