How Is Technology Changing Sleep Testing in Melbourne?
Modern sleep testing Melbourne facilities now deliver diagnostic precision that was unimaginable a decade ago. Accurate diagnosis of sleep disorders directly impacts treatment success rates and prevents serious health complications ranging from cardiovascular disease to mental health deterioration.
Melbourne residents increasingly turn to advanced sleep technology for answers to persistent sleep problems. The shift from traditional hospital-only testing to sophisticated home-based diagnostics has made professional sleep assessment accessible to thousands who previously delayed seeking help.
The Technology Behind Modern Sleep Testing Melbourne Residents Now Rely On
The Technology Behind Modern Sleep Testing Melbourne Residents Now Rely On addresses conditions spanning the severity spectrum:
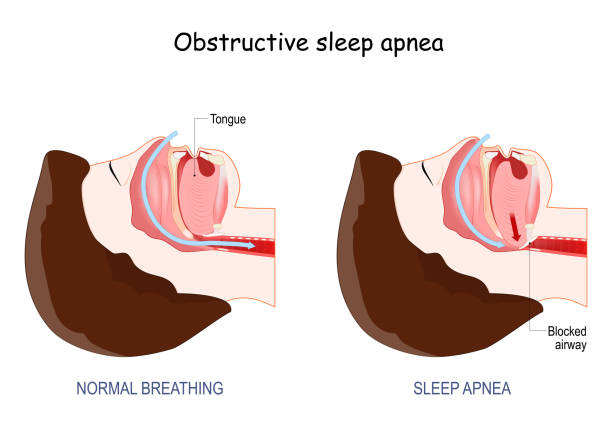
- Snoring: Often dismissed as merely disruptive, yet potentially indicating partial airway obstruction
- Obstructive Sleep Apnea (OSA): A serious condition where breathing repeatedly stops during sleep, starving the brain and body of oxygen
- Sleep movement disorders: Conditions affecting rest quality through involuntary physical activity
These disorders share common symptoms—daytime fatigue, concentration difficulties, mood changes—making technological differentiation essential for appropriate treatment.
What Are the Key Technologies Used in Modern Sleep Testing?
Modern sleep testing relies on two primary approaches: in-home sleep testing and comprehensive polysomnography conducted in clinical settings. In-home testing has transformed how Melbourne residents access diagnostic services by eliminating the need for overnight hospital stays. Patients receive portable monitoring equipment that records essential sleep data in their own bedrooms, making the process less disruptive and more representative of typical sleep patterns.
Physiological Monitoring Tools
Physiological monitoring tools capture multiple data streams simultaneously during sleep studies. These sophisticated sensors track:
- Oxygen saturation levels through pulse oximetry, revealing how effectively the body maintains adequate oxygen during sleep
- Airflow patterns via nasal sensors that detect breathing interruptions or reductions
- Heart activity monitored through electrocardiogram (ECG) technology, identifying irregular rhythms or stress responses
- Chest and diaphragm movements that show respiratory effort
- Brain wave activity using electroencephalogram (EEG) sensors
- Muscle tone measured by electromyogram (EMG) devices
- Eye movements tracked through electrooculogram technology
Hospital-Based Polysomnography
Hospital-based polysomnography serves patients with complex or unclear presentations. These overnight studies provide the most comprehensive diagnostic picture available, with technicians monitoring real-time data throughout the night. The controlled environment allows for immediate intervention if safety concerns arise and enables detailed observation of sleep architecture across multiple cycles.
Choosing Between Home and Hospital Testing
The choice between home and hospital testing depends on symptom severity, medical history, and the suspected condition. Simple cases of suspected obstructive sleep apnea often qualify for home testing, while patients with comorbid conditions, unusual symptoms, or previous inconclusive results benefit from the enhanced monitoring capabilities of laboratory polysomnography. Both approaches generate detailed physiological data that clinicians analyze to identify specific sleep disorders and their severity.
Why Is In-Home Sleep Testing Popular Among Melbourne Residents?
In-home sleep testing eliminates the need for hospital visits, allowing patients to sleep in their own beds while sophisticated sensors collect diagnostic data. This non-invasive sleep study approach has transformed how Melbourne residents access sleep disorder diagnosis, removing the anxiety and disruption associated with unfamiliar clinical environments.
The technology relies on carefully calibrated sensors that patients attach themselves before bedtime. Oximetry clips monitor oxygen saturation levels throughout the night, detecting critical drops that signal breathing interruptions. Chest and abdominal bands measure respiratory effort, while nasal airflow sensors track breathing patterns with precision.
Brain activity monitoring through EEG electrodes captures sleep stages and arousal patterns without causing discomfort. EMG sensors placed on the chin and legs record muscle movements, identifying conditions like periodic limb movement disorder or REM sleep behavior disorder. Electrooculogram sensors near the eyes track rapid eye movements, essential for distinguishing between sleep stages and diagnosing specific disorders.
Patient comfort drives adoption rates across Melbourne. Sleeping in familiar surroundings produces more representative data than a single night in a clinical setting. Many patients report better sleep quality at home despite wearing monitoring equipment, leading to more accurate diagnostic results.
The real-world data collection advantage cannot be overstated. Home testing captures natural sleep patterns influenced by typical bedroom conditions—temperature, noise levels, partner presence, and usual bedtime routines. This authentic environmental context helps clinicians understand how sleep disorders manifest in patients’ daily lives, enabling more targeted treatment recommendations.
Cost-effectiveness and accessibility make in-home testing the preferred first-line diagnostic tool for suspected sleep apnea and related conditions throughout Melbourne’s healthcare system.
What Role Do Hospital-Based Sleep Studies Play in Diagnosing Complex Sleep Disorders?
Overnight polysomnography in specialized sleep labs becomes essential when home testing results prove inconclusive or symptoms suggest complicated sleep disorders. These hospital-based studies capture a complete picture of sleep physiology that home devices cannot always provide.
Comprehensive monitoring in clinical settings tracks multiple physiological systems simultaneously:
- Brain wave patterns through advanced EEG technology reveal sleep stage transitions and neurological disruptions
- Cardiac rhythms detect irregular heart patterns that may indicate serious cardiovascular complications
- Respiratory effort measurements distinguish between central and obstructive apnea types
- Limb movements identify periodic leg movements or REM sleep behavior disorders
Specialized sleep labs employ trained technologists who observe patients throughout the night, adjusting equipment and noting behaviors that automated systems might miss. This human element proves invaluable when diagnosing conditions like narcolepsy, parasomnias, or treatment-resistant insomnia.
Hospital studies work alongside home testing rather than replacing it. Patients typically start with convenient home assessments, then progress to laboratory polysomnography when initial results raise questions or symptoms persist despite treatment. This tiered approach ensures Melbourne residents receive appropriate diagnostic intensity while maintaining healthcare efficiency and cost-effectiveness for straightforward cases.

Which Portable Devices Support Ongoing Sleep Disorder Treatment?
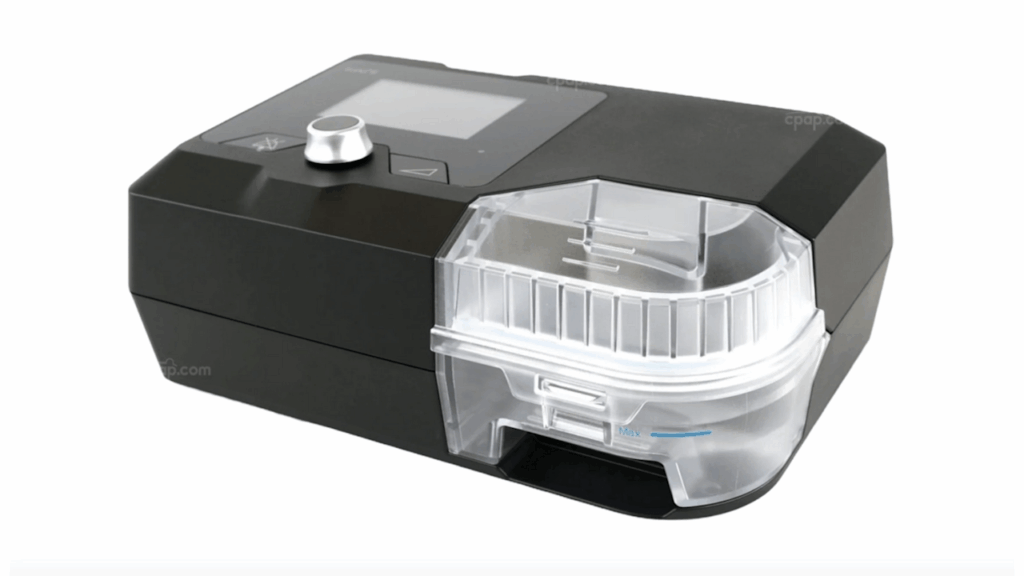
CPAP machines are still the best option for treating obstructive sleep apnea. These devices deliver continuous pressurized air through a mask, keeping airways open throughout the night and preventing the repeated breathing interruptions that characterize OSA. Modern CPAP units are compact, whisper-quiet, and equipped with humidifiers to enhance comfort during extended use.
The technology tracks usage patterns and treatment efficacy, allowing clinicians to adjust pressure settings remotely. Patients typically notice immediate improvements in daytime alertness and energy levels once therapy begins.
Mandibular advancement splints offer an alternative solution for individuals with snoring or mild to moderate sleep apnea. These custom-fitted mouthguard-style devices work by gently repositioning the lower jaw forward during sleep, which increases the space in the airway and reduces tissue vibration.
Portable treatment devices provide several distinct advantages:
- Compact design makes them ideal for travel and business trips
- Silent operation eliminates noise concerns for bed partners
- Non-invasive approach appeals to patients who find masks uncomfortable
- Custom fitting ensures optimal positioning and effectiveness
Dental sleep medicine specialists create these appliances using precise measurements and impressions. Regular follow-up appointments allow for adjustments that maximize therapeutic benefits while maintaining jaw comfort. Many Melbourne residents prefer these devices for their discretion and ease of use compared to traditional CPAP therapy.
How Does a Multidisciplinary Approach Enhance Sleep Disorder Care in Melbourne?
Multidisciplinary sleep clinics Melbourne facilities bring together specialized professionals who address sleep disorders from multiple angles simultaneously. A single sleep physician cannot tackle the psychological, respiratory, and lifestyle factors that often contribute to poor sleep quality.
Modern clinics like SleepDoctors Melbourne assemble teams that typically include:
- Sleep psychologists who specialize in behavioral interventions
- Respiratory specialists trained in airway management
- Medical scientists who analyze complex sleep study data
- Sleep physicians who coordinate treatment strategies
Cognitive behavioral therapy for insomnia (CBT-I) forms a cornerstone of psychological intervention at these facilities. This evidence-based therapy helps patients identify and modify thoughts and behaviors that interfere with sleep. Sleep psychologists deliver CBT-I alongside mindfulness techniques, teaching patients to manage anxiety and racing thoughts that prevent restful sleep.
The integration happens through personalized treatment plans built from detailed sleep study results. A patient’s test data might reveal both physical airway obstruction and anxiety-driven insomnia. The respiratory specialist addresses the physical component with CPAP therapy or oral appliances, while the psychologist implements CBT-I to resolve behavioral patterns.
Medication management adds another layer when appropriate. Sleep physicians prescribe targeted medications based on specific sleep architecture disruptions identified in testing, avoiding the one-size-fits-all approach that often fails patients.
This collaborative model ensures that treatment addresses root causes rather than symptoms alone. Team members review cases together, adjusting interventions as new data emerges from follow-up testing. Patients benefit from coordinated care that considers their complete sleep health picture, leading to more sustainable improvements in sleep quality and daytime functioning.
How Is Advanced Data Analysis Used to Differentiate Between Snoring and Serious Conditions Like OSA?
Clinical data interpretation transforms raw sleep study measurements into actionable medical insights. Experienced clinicians at Melbourne sleep centers analyze complex datasets that include breathing patterns, heart rhythms, and brain activity to distinguish harmless snoring from life-threatening conditions.
The Role of Oxygen Desaturation Analysis
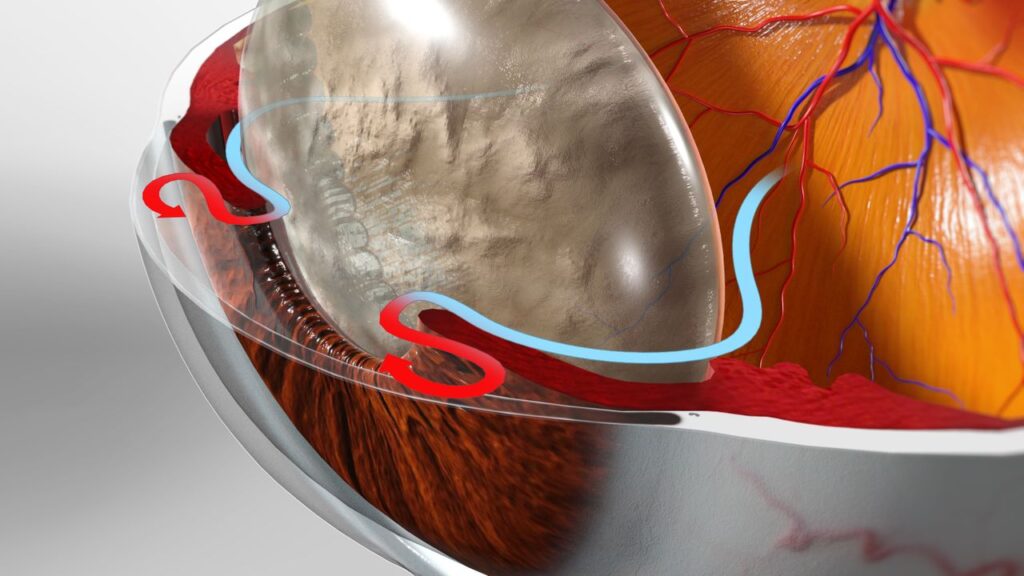
Oxygen desaturation analysis serves as a critical diagnostic marker in this process. When oxygen levels drop repeatedly during sleep—often falling below 90% saturation—it signals that the brain and muscles are experiencing significant stress. These desaturation events occur when airways collapse during sleep, forcing the body into micro-arousals that fragment rest quality.
Understanding the Health Risks of OSA
The health risks of OSA extend far beyond daytime fatigue. Untreated obstructive sleep apnea creates a cascade of physiological problems:
- Cardiovascular complications including hypertension, irregular heart rhythms, and increased stroke risk
- Mental health deterioration with higher rates of depression and anxiety
- Gastroesophageal reflux disease (GERD) exacerbation
- Metabolic dysfunction affecting blood sugar regulation
The Role of Skilled Sleep Specialists
Skilled sleep specialists examine the frequency and duration of these oxygen drops alongside other physiological markers. A patient experiencing 15 or more desaturation events per hour meets diagnostic criteria for moderate OSA, requiring immediate intervention. This precision in The Technology Behind Modern Sleep Testing Melbourne Residents Now Rely On ensures appropriate treatment pathways are selected based on severity levels rather than symptoms alone. Click here to get 2025 guide to finding a bulk-bill sleep study Hobart patients can rely on.
What Technologies Are Used to Monitor Treatment Effectiveness Over Time?
Actigraphy devices provide objective evaluation methods that track patient progress long after initial diagnosis. These wrist-worn sensors continuously record movement patterns during sleep, creating detailed data sets that reveal whether CPAP therapy, oral appliances, or behavioral interventions are delivering expected results.
The technology works by detecting micro-movements throughout the night. When treatments succeed, patients experience fewer sleep disruptions, reflected in more stable movement patterns. The devices distinguish between restful sleep and periods of fragmentation that indicate ongoing problems requiring intervention adjustments.
Treatment monitoring technology has transformed follow-up care from subjective patient reports to data-driven assessments. Melbourne sleep specialists now receive weeks or months of objective sleep-wake data, allowing them to identify subtle patterns invisible during single-night studies. This extended monitoring captures night-to-night variability that influences treatment decisions.
The continuous nature of actigraphy monitoring proves particularly valuable for:
- Detecting treatment compliance issues – devices reveal whether patients consistently use prescribed therapies
- Identifying effectiveness plateaus – data shows when initial improvements stall, signaling the need for protocol modifications
- Measuring response to therapy adjustments – clinicians compare pre- and post-adjustment data to validate changes
- Tracking seasonal or lifestyle impacts – long-term monitoring reveals how external factors affect sleep quality
Sleep clinics integrate actigraphy data with periodic symptom assessments and device download information from CPAP machines. This multi-source approach creates comprehensive treatment profiles, enabling specialists to fine-tune interventions based on real-world performance rather than laboratory conditions alone. The technology shifts sleep disorder management from reactive problem-solving to proactive optimization.

What’s Next for Sleep Testing Technology in Melbourne?
The future of sleep testing Melbourne residents can expect centers on artificial intelligence integration and miniaturized sensors that deliver even more precise diagnostics. Machine learning algorithms are already being developed to detect subtle breathing pattern changes that human analysis might miss, enabling earlier intervention for conditions like OSA.
Wearable technology continues evolving beyond basic actigraphy. Next-generation devices will combine continuous blood oxygen monitoring, heart rate variability analysis, and sleep stage detection in single, unobtrusive units. These advancements mean patients receive real-time feedback about their sleep quality without visiting clinics repeatedly.
Telemedicine platforms are transforming how Melbourne sleep specialists interpret data and adjust treatments remotely. Patients upload their overnight readings directly to cloud-based systems where clinicians review results within hours rather than weeks. This rapid response cycle accelerates the path to improving quality of life through technology.
The Technology Behind Modern Sleep Testing Melbourne Residents Now Rely On will increasingly focus on predictive analytics—identifying sleep disorder risks before symptoms become severe, shifting from reactive treatment to proactive prevention.